Studies have shown that musculoskeletal disorders are among the top three reasons why dentists seek medical attention, and these disorders can lead to long-term disability and even early retirement.
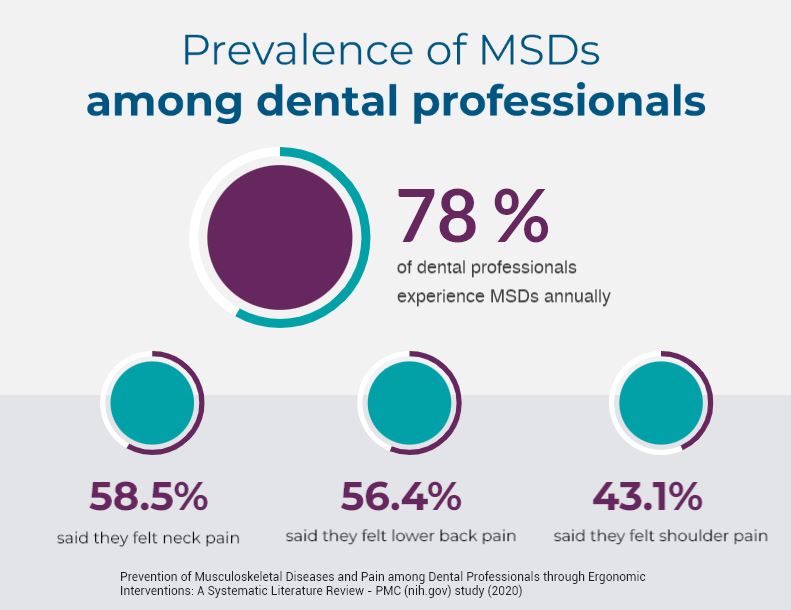
As a dental professional, there is a good chance you have experienced an MSD in your career – a recent study found that an astounding 78% of all dental professionals report having had them (4) – along with the unforgettable symptoms associated including pain, stiffness, numbness, tingling, weakness or swelling in the affected areas.
In this article, we’ll dive into the world of MSDs and their impact on dental professionals. We’ll explore common types of MSDs, their causes and symptoms. By understanding how MSDs can affect your body and career, you can take steps to protect yourself and continue providing excellent care to your patients. So let’s get started!
The prevalence of musculoskeletal disorders in dentistry is especially concerning given the fact that most dental professionals are expected to work long hours and are often seated in awkward positions for long periods of time.
According to a study published in the Journal of Occupational Health, dentists and dental hygienists are at high risk of developing MSDs due to prolonged periods of standing, awkward postures, and repetitive motions such as gripping dental instruments (1). These physical demands can put stress on the muscles and joints, leading to pain and discomfort that can ultimately affect job performance and quality of life.
Research published in the International Journal of Preventive Medicine found additional factors that could contribute to work-related MSDs including (3):
Working Hours – Those who work more than 12 hours per day have a higher prevalence of work-related MSDs.
Job changes – Changing jobs is another predictor that negatively correlates with MSDs. Not surprisingly, dental staff experiencing MSDs are more apt to frequently change jobs due to work-related pain.
And dental hygienists find themselves in even greater risk of MSDs because of the type of work they do in a dental practice. This is due to procedures that involve precise, repetitive motions, as well as awkward and static postures. MSDs affect and cause a range of injuries in the wrist (carpal tunnel), elbow (Epicondylitis), and the shoulders, along with the back and hips.
Because of the nature of clinical dentistry—static posture, precise and repetitive motions, long work hours, and suboptimal ergonomics—all members of the clinical team are at risk for MSDs.
As the pain escalates, absenteeism-related production losses, worker’s comp claims and personal treatment costs further erode practice profitability. In fact, MSDs can become so severe that, in some cases, they lead to premature retirement for dental professional (5).
Fortunately, MSDs can be preventable through the use of ergonomic intervention.
In an article written by Dimensions of Dental Hygiene, to help prevent MSDs it is important for dental professionals to take breaks throughout the workday, maintain good posture, and use ergonomic equipment designed specifically for the dental profession (2). By taking these steps, dental professionals can reduce their risk of developing MSDs and continue to provide high-quality care to their patients.
Your team is the integral component of your practice’s success and every member – especially the hygienist – should seek clinical equipment that can reduce muscle workload and its duration. So, if we know all this, why do MSDs continue to be such a pervasive and nagging problem in the dental profession? For the most part, it’s human nature. Practices tend to look at expenditures from the top down. Often purchasing big-ticket teeth whitening systems, digital x-ray equipment and other solutions are the priority as they can be revenue generators, while ergonomic equipment like seating takes a back seat. Why replace something that is still in working order, right? But upgrading to ergonomic equipment now can help save you much more down the road.
If you would like to discuss your practice’s health and what seating is right for your team, reach out to us at 262-251-9530 or fill out a request a quote on our website.
Other articles in our dental seating series:
Article 2: Tips to Choosing the Right Dental Stool
Article 3: Don’t Settle for Cheap: Invest in Quality Dental Stools for Maximum Comfort and Health
(1) Moodley R, Naidoo S, Wyk JV. The prevalence of occupational health-related problems in dentistry: A review of the literature. J Occup Health. 2018 Mar 27;60(2):111-125. doi: 10.1539/joh.17-0188-RA. Epub 2017 Dec 6. PMID: 29213011; PMCID: PMC5886878.
(2) Wilkinson B, Erenfeld H, Coplen A. Basic Prevention and Management of Common Musculoskeletal Disorders. Dimensions of Dental Hygiene. 2022 Jan 31. dimensionsofdentalhygiene.com/article/basic-prevention-and-management-of-common-musculoskeletal-disorders/
(3) Alzayani MK, Salama KF, Zafar M. Work-related Musculoskeletal Disorders Among Dental Staff in Armed Force Hospital in Dhahran, Saudi Arabia. Int J Prev Med. 2021 Sep 29;12:119. doi: 10.4103/ijpvm.IJPVM_136_20. PMID: 34760130; PMCID: PMC8551768.
(4) Lietz J, Ulusoy N, Nienhaus A. Prevention of Musculoskeletal Diseases and Pain among Dental Professionals through Ergonomic Interventions: A Systematic Literature Review. Int J Environ Res Public Health. 2020 May 16;17(10):3482. doi: 10.3390/ijerph17103482. PMID: 32429439; PMCID: PMC7277669.
(5) Lietz J, Ulusoy N, Nienhaus A. Prevention of Musculoskeletal Diseases and Pain among Dental Professionals through Ergonomic Interventions: A Systematic Literature Review. Int J Environ Res Public Health. 2020 May 16;17(10):3482. doi: 10.3390/ijerph17103482. PMID: 32429439; PMCID: PMC7277669.
Explore Brewer dental seating
Whether you want traditional, saddle or assistant seating - we have the perfect stool for you.




